Ever had that bloated feeling after lunch that just won’t go away? Or woken up in the middle of the night with heartburn so bad you thought you were having a heart attack? You’re not alone. About 1 in 4 people in the UK deal with digestive symptoms like these every week. Yet most of us still don’t know what’s really going on inside our guts. Gastro health isn’t just about avoiding spicy food or taking antacids. It’s about understanding how your stomach, intestines, and gut bacteria work together - and what happens when they don’t.
What Exactly Is Gastro Health?
Gastro health refers to the overall condition of your digestive system - from your mouth to your anus. It includes how well you break down food, absorb nutrients, move waste out of your body, and keep harmful bacteria in check. A healthy gut doesn’t mean you never get an upset stomach. It means your system recovers quickly, doesn’t send constant warning signals, and supports your immune system and even your mood.
Many people think gastro health is just about acid reflux or constipation. But it’s deeper than that. Your gut contains trillions of bacteria - more than the number of cells in your whole body. These microbes help digest fibre, make vitamins like B12 and K, and even send signals to your brain. When they’re out of balance, you might feel tired, anxious, or get frequent infections. That’s why gastro health affects more than just your belly.
Why Do I Get Bloating After Eating?
Bloating isn’t normal - even if everyone says it is. If you feel swollen, tight, or distended after meals, something’s off. The most common cause? Gas buildup from undigested food. But why isn’t your body digesting it properly?
- Swallowing air - Talking while eating, chewing gum, or drinking through a straw can make you swallow extra air. That air ends up in your gut and causes puffiness.
- FODMAPs - These are short-chain carbs found in onions, garlic, beans, apples, and wheat. They’re fermented by gut bacteria, creating gas. Around 75% of people with IBS see big improvements cutting these out.
- Low stomach acid - Most people assume bloating comes from too much acid. But low acid is actually more common. Without enough acid, food sits in your stomach too long, ferments, and bloats you up.
Try this: Eat slowly. Put your fork down between bites. Drink water before meals, not during. If bloating sticks around for more than a few days, keep a food diary. Note what you ate, when you felt bloated, and how bad it was. Patterns will show up fast.
Is Acid Reflux Just from Spicy Food?
No. While chili peppers and pizza can trigger it, the real culprit is often a weak lower oesophageal sphincter - the muscle that keeps stomach acid from flowing back up. This muscle can weaken from:
- Being overweight - extra belly pressure pushes acid upward
- Eating large meals - your stomach gets too full
- Lying down after eating - gravity stops working in your favour
- Chronic stress - it slows digestion and relaxes the sphincter
Some surprising triggers? Coffee, chocolate, mint, and even plain water if you drink a lot right before bed. Over-the-counter antacids give quick relief, but they don’t fix the root cause. Long-term use can even make things worse by lowering stomach acid too much.
Try this instead: Eat your last meal at least 3 hours before bed. Sleep with your head slightly raised. Lose even 5% of your body weight if you’re carrying extra pounds - it cuts reflux episodes by over half in most people.

What’s the Deal with IBS?
IBS - Irritable Bowel Syndrome - is one of the most common gut diagnoses. But it’s not a disease. It’s a label for a group of symptoms: cramping, bloating, diarrhoea, constipation, or switching between them - with no clear physical cause.
Doctors used to say IBS was "all in your head." That’s outdated. Brain-gut connections are real. Stress, trauma, and even past infections can change how your gut nerves respond. The good news? IBS is manageable.
The low-FODMAP diet is backed by over 100 clinical studies. It doesn’t mean cutting out all healthy foods. It means temporarily removing high-gas foods, then slowly adding them back to find your personal triggers. Most people find they can eat some onions, apples, or beans again - just not all at once.
Probiotics also help. Not all of them, though. Look for strains like Bifidobacterium infantis 35624 or Lactobacillus plantarum 299v. These have been tested specifically for IBS. Generic store-bought yoghurts? Usually not enough.
Can Gut Health Affect My Mood?
Yes. Your gut makes 90% of your body’s serotonin - the chemical that helps you feel calm and happy. When your gut lining is inflamed or your bacteria are out of balance, serotonin production drops. That’s why people with chronic digestive issues are 2-3 times more likely to have anxiety or depression.
It works both ways. Stress doesn’t just make your stomach hurt - it changes your gut bacteria. In one study, people under chronic stress had 30% less of the beneficial Lactobacillus strains. Their gut became more permeable - letting toxins leak into the bloodstream, which triggered inflammation.
Fixing your gut doesn’t mean you’ll stop being anxious overnight. But many patients report clearer thinking, less brain fog, and fewer panic attacks after 6-8 weeks of dietary changes and stress reduction.
Do I Need to Take Probiotics?
Not necessarily. Most healthy people get enough good bacteria from food. Fermented foods like sauerkraut, kimchi, kefir, miso, and plain yoghurt with live cultures are better than pills. They come with fibre, enzymes, and other nutrients that help the bacteria survive.
Probiotic supplements can help if:
- You’ve just finished a course of antibiotics
- You have IBS or antibiotic-associated diarrhoea
- You’ve had a gut infection in the past year
But not all probiotics are equal. A 2023 review of 18 studies found that only 3 strains consistently helped: Lactobacillus rhamnosus GG, Bifidobacterium lactis HN019, and Saccharomyces boulardii. Look for products with at least 10 billion CFUs and that list the exact strain names on the label.
And here’s the catch: probiotics don’t stay in your gut forever. You need to keep eating them regularly. One dose won’t fix years of poor diet.
What Should I Eat for Better Gastro Health?
Forget detoxes and juice cleanses. Real gut healing comes from consistent, simple habits:
- Fibre - Aim for 30g a day. Oats, lentils, chickpeas, broccoli, and apples are great. Most people get less than half that.
- Prebiotics - These are food for your good bacteria. Garlic, leeks, asparagus, bananas, and chicory root are top sources.
- Healthy fats - Omega-3s from salmon, walnuts, and flaxseeds reduce gut inflammation.
- Hydration - Drink water throughout the day. Dehydration slows digestion and leads to hard stools.
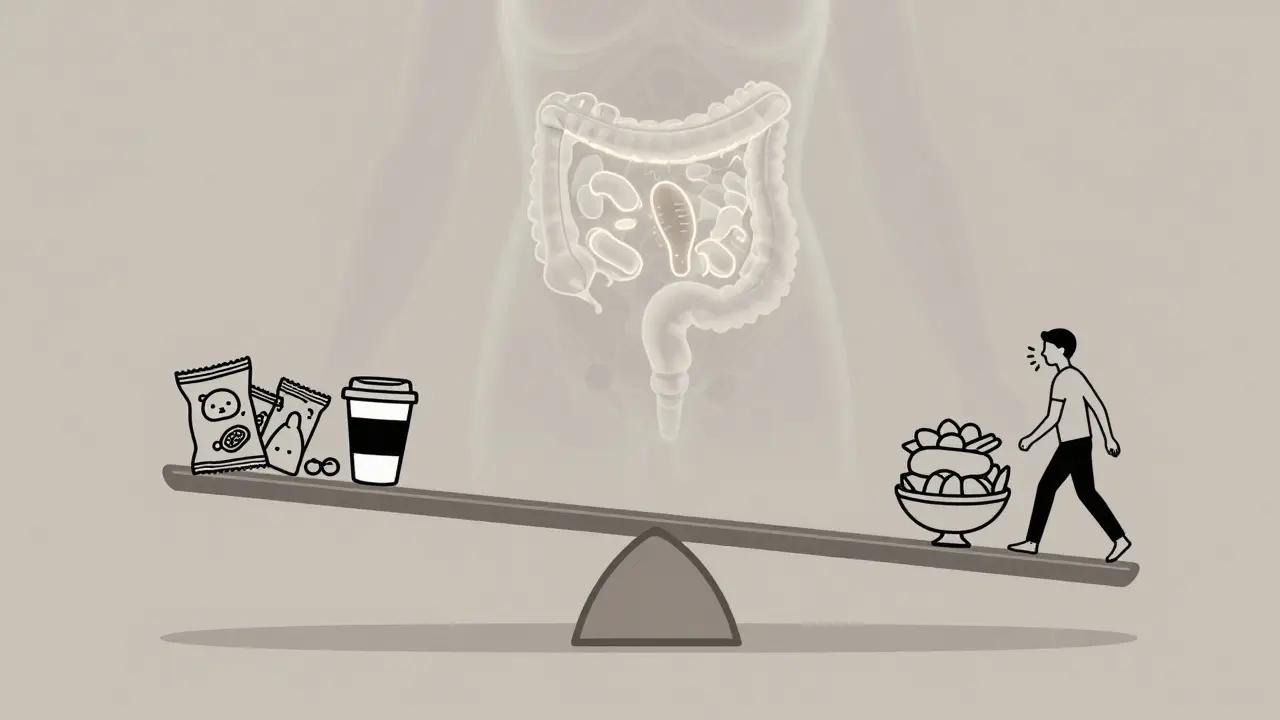
- Limit ultra-processed foods - Things like sugary cereals, packaged snacks, and ready meals contain emulsifiers and artificial sweeteners that harm gut bacteria.
Try the 80/20 rule: Eat whole, unprocessed foods 80% of the time. Leave room for the other 20% without guilt. Perfection isn’t the goal - consistency is.
When Should I See a Doctor?
Most digestive issues aren’t serious. But some red flags need checking:
- Unexplained weight loss
- Blood in stool or black, tarry stools
- Swallowing pain or trouble swallowing
- Severe, persistent pain that wakes you up at night
- Family history of bowel cancer or IBD
If you’re over 50 and your digestion has changed suddenly - even mildly - get a check-up. Bowel cancer is treatable if caught early. Don’t wait for "it gets worse."
Also, if you’ve tried dietary changes for 6-8 weeks and nothing’s improved, see a gastroenterologist. You might need tests for celiac disease, SIBO (small intestinal bacterial overgrowth), or inflammatory bowel disease.
Can I Fix My Gut Without Medication?
Yes - and most people should try before reaching for pills. Lifestyle changes are the most powerful tools you have.
Here’s what works:
- Chew your food slowly - aim for 20-30 chews per bite.
- Manage stress with daily breathing exercises - even 5 minutes helps.
- Move your body - walking after meals improves digestion more than you think.
- Sleep 7-8 hours - poor sleep messes with your gut rhythm.
- Stop smoking and cut back on alcohol - both damage the gut lining.
It’s not about doing everything at once. Pick one thing - maybe chewing slower or drinking more water - and stick with it for 2 weeks. Then add another. Small steps build lasting change.
Is bloating always a sign of a serious problem?
No, occasional bloating after meals is normal, especially after eating gas-producing foods like beans or cabbage. But if it’s constant, painful, or accompanied by weight loss, blood in stool, or vomiting, it could signal something more serious like IBS, SIBO, or even cancer. Track your symptoms and see a doctor if they persist beyond two weeks.
Can stress really cause stomach problems?
Absolutely. Stress activates your fight-or-flight response, which shuts down digestion. This can lead to cramps, bloating, diarrhoea, or constipation. Chronic stress also changes your gut bacteria and increases inflammation. Managing stress through breathing, walking, or talking to someone can improve gut symptoms as much as dietary changes.
Are probiotic supplements better than fermented foods?
Not necessarily. Fermented foods like kimchi, kefir, and sauerkraut offer a wider variety of live cultures and nutrients that help them survive in your gut. Supplements can be useful if you need specific strains for conditions like IBS or after antibiotics, but they’re not a magic fix. Most people benefit more from eating real food than popping pills.
Why do I get heartburn when I eat chocolate?
Chocolate contains methylxanthines, which relax the lower oesophageal sphincter - the muscle that keeps stomach acid from rising. Even small amounts can trigger reflux in sensitive people. It’s not just spicy food - chocolate, coffee, mint, and alcohol are common triggers. Cutting them out for a few weeks often reveals how much they’re affecting you.
Does drinking water help digestion?
Yes, but timing matters. Drinking too much water during meals can dilute stomach acid, making digestion slower. Better to drink water 20-30 minutes before meals and wait an hour after. Staying hydrated overall helps move food through your intestines and prevents constipation. Aim for 1.5-2 litres a day, more if you’re active.





