Your body can process stress even when words won’t cooperate. That’s the core promise here: you can feel better by making, moving, and sounding things out. This isn’t a hobby-in-disguise. It’s a clinical approach that uses the arts to support mental health, physical recovery, and everyday resilience. Expect a grounded guide-what it is, who it helps, how it works, and simple ways to begin at home or with a therapist.
TL;DR
- Creative arts therapies are clinical, evidence-backed approaches using art, music, movement, and drama to support mental and physical health.
- They help with stress, anxiety, depression, trauma, pain, and chronic illness; they also support neurodiversity and aging.
- Getting started: pick a modality that matches your goals, try a 20-minute home routine, and consider one session with a credentialed therapist.
- What to expect: you don’t need talent; the focus is process, not product. Safety and choice matter more than “being good at it.”
- Measure progress with simple markers: sleep, mood, energy, pain, social connection, and daily function.
What It Is, How It Helps, and Who It’s For
When you hear “therapy,” you might picture a couch and a lot of talking. Here, the arts do the heavy lifting. In creative arts therapies, credentialed clinicians use visual art, music, movement, and drama to help you process emotions, regulate your nervous system, and build coping skills. You don’t need talent. You need curiosity and consent.
Quick map of modalities:
- Art therapy: drawing, painting, collage, clay, or mixed media to express and explore feelings, memories, and body sensations.
- Music therapy: listening, playing, singing, songwriting, and rhythm to reduce pain and anxiety, improve mood, and support rehab.
- Dance/movement therapy: movement, breath, and posture to process emotions and improve regulation, mobility, and presence.
- Drama therapy: role-play, storytelling, and improvisation to safely try new behaviors and rewrite stuck narratives.
- Expressive arts therapy: integrative-shifting between art, sound, movement, and words as needed.
What the research actually says:
- World Health Organization (2019) published a scoping review of 900+ studies concluding the arts can support prevention and management of mental and physical health conditions across the lifespan.
- Cochrane reviews (Aalbers et al., 2017; updates through 2021) found music therapy added to standard care reduces depressive symptoms more than standard care alone.
- The Lancet (Hole et al., 2015) reported that perioperative music reduces pain, anxiety, and opioid use after surgery.
- Meta-analyses (Koch et al., 2019) show dance/movement therapy produces moderate improvements in depression and anxiety.
- NICE guidance on psychosis and schizophrenia recommends arts therapies to help with negative symptoms and engagement (2014, updated 2020).
- Systematic reviews in dementia care point to music and movement improving agitation and social connection, while visual arts activities support identity and purpose.
Why it works (plain terms):
- Bottom-up regulation: rhythm, breath, and movement calm the autonomic nervous system when words can’t. That’s why steady beats and slow exhale cues help panic.
- Embodied processing: many emotions live in the body. Moving, shaping, humming-these bridge feelings and meaning.
- Agency and play: choosing a color, tempo, or role builds confidence and flexibility. Healthy play is serious nervous system work.
- Relationship: the therapist offers attunement and safety. That co-regulation trains your body to settle and engage.
Who benefits most:
- Stress, burnout, and sleep issues: structured creative routines ease rumination and help downshift.
- Anxiety and depression: music, movement, and visual expression reduce symptoms and boost motivation.
- Trauma: nonverbal routes offer safe distance and control while integrating difficult memories.
- Chronic pain and illness: rhythm and breath lower perceived pain; art and drama rebuild identity and coping.
- Neurodiversity: rhythm and movement can support regulation, communication, and sensory integration.
- Aging and dementia: music unlocks memory and connection when language declines; art sustains meaning.
Common myths to drop now:
- “I can’t draw/sing/dance.” Good. Talent isn’t the point. The process heals, not the polish.
- “It’s not real therapy.” These are clinical disciplines with research, codes of ethics, and formal training.
- “It’s only for kids.” Adults often benefit even more because they’re stuck in their heads; the arts pull them back into their bodies.
How to Start: Step-by-Step, At Home or With a Therapist
If you just want to feel calmer and think clearer, start small. You can try a safe 20-minute routine at home today. If your history includes trauma, severe depression, psychosis, or eating disorders, consider pairing with a credentialed therapist for safety and pacing.
Job 1: Choose the right modality for your goal
- High anxiety or panic: try music (steady beats around 60-80 BPM), humming, or slow sway; or simple repetitive drawing (spirals, lines).
- Low mood and flat energy: try drumming along to upbeat tracks, color blocking with bold paints, or a short movement improvisation.
- Night-time stress: 6 breaths per minute with soft humming, then gentle sketching or collage before bed.
- Pain management: rhythm-based breathing and music before and during painful tasks; brief art journaling after.
- Interpersonal stress: drama therapy exercises (role reversal, letter-to-self, imagined dialogues) can unlock stuck scripts.
Job 2: Set up a simple 20-minute home practice (no talent required)
- Arrival (2 minutes): sit, feet grounded. Inhale through the nose 4 counts, exhale 6-8 counts. Notice 3 things you see, 2 you hear, 1 you feel.
- Core activity (12-14 minutes): pick one:
- Art: draw repeating shapes with one color for 3 minutes; switch color and shape each song change. If emotions show up, pause and name them on the page.
- Music: choose 3 songs-calm, steady, uplift. Hum or tap along. Let your breath sync to the beat.
- Movement: set a timer for 8 minutes. Move only shoulders and hands for 2 minutes, add torso for 2, add legs for 2, free move for 2. Keep it gentle.
- Drama/writing: write an inner monologue in third person for 5 minutes (“She wakes up…”) then read it out loud in a warm, kind voice.
- Wrap (4 minutes): jot down 3 words for mood, 2 body sensations, 1 next tiny step (e.g., “drink water,” “open window”).
Job 3: Plan a 4-week starter track
- Week 1-Regulate: do the 20-minute routine 3 times. Track sleep, stress (0-10), and energy (0-10).
- Week 2-Express: add 1 deeper prompt (e.g., draw “what my tension looks like” or drum for 5 minutes before journaling). Note any shifts in mood.
- Week 3-Connect: invite a friend or join a community class for one session. Notice motivation and belonging.
- Week 4-Reflect: keep what works, drop what doesn’t. Decide if you want to book a therapist-led session.
Job 4: Work with a credentialed therapist
- Credentials to look for (varies by country): RCAT (Registered Canadian Art Therapist), MTA (Accredited Music Therapist in Canada), R-DMT or BC-DMT (Dance/Movement Therapy), RDT (Registered Drama Therapist). Many also hold counseling or psychology credentials.
- First session: expect goal setting, consent, and a gentle activity to gauge comfort and needs. You control the pace.
- Cost and coverage: in Canada, extended health benefits often cover sessions with registered therapists; some clinics offer sliding scales and group programs.
- Remote options: virtual sessions work well for music and art; movement and drama also adapt with camera framing and safety check-ins.
Job 5: Safety first-set guardrails
- Pick activities that are slow, predictable, and adjustable. This is not exposure therapy unless planned with a clinician.
- Stop if you feel dizzy, numb, or overwhelmed. Ground, hydrate, and switch to a neutral task (fold laundry, step outside).
- Keep a “reset” list nearby: 5-4-3-2-1 senses scan, cold water on wrists, gentle wall push, two-hand tapping on thighs.
- If you have active trauma symptoms, suicidal thoughts, or eating-disorder urges, work with a qualified therapist.
Helpful heuristics (quick decision rules):
- When in doubt, add rhythm. Steady, simple beats regulate faster than complex patterns.
- Match first, then lead. Start with your current energy or mood; shift the tempo or color slowly.
- Short and frequent beats long and rare. Three 15-20 minute sessions per week beats one long session.
- Keep choices shallow at first. Limit to two options (blue or green; slow or medium tempo) to reduce overwhelm.

Make It Stick: Examples, Checklists, FAQs, and Troubleshooting
Real-life scenarios help you see what’s possible. Here are a few snapshots and then the practical tools to keep you going.
Example 1: The Sunday Scaries
- Goal: ease work anxiety before Monday.
- Plan: 18-minute music-and-mark-making. Two slow tracks (60-70 BPM) then one brighter track (80-90 BPM). While listening, draw repeating lines on scrap paper. On the last track, write three action words for Monday (“email,” “draft,” “stretch”).
- Result: heart rate drops, a plan appears, sleep improves.
Example 2: Pain Flare Day
- Goal: reduce pain intensity during afternoon slump.
- Plan: 6 rounds of 4-6 breathing while humming; 6 minutes of gentle chair movement with a metronome at 70 BPM; 4 minutes sketching a simple gradient from dark to light.
- Result: pain rating drops from 7/10 to 5/10, mood steadies, you can make dinner.
Example 3: Post-Conflict Reset
- Goal: reconnect after an argument.
- Plan: drama therapy at home-write a short “script” where each person gets 60 seconds to voice their view while the other repeats back key words. Close with 2 minutes of synchronized breathing and a shared playlist pick.
- Result: less defensiveness, clearer needs, faster repair.
Example 4: Brain Fog at Work
- Goal: sharpen focus midafternoon.
- Plan: two-minute micro-move (wrists, shoulders, neck), 90 seconds of finger tapping to a steady beat, then a three-color sticky-note sketch of your top task. Timer for 15 minutes, go.
- Result: task initiation kicks in, you finish a chunk without spiraling.
Readiness checklist (five quick yes/no):
- Do I have 20 minutes without interruption today?
- Do I have a safe, seated option if standing movement spikes symptoms?
- Do I have two simple choices ready (e.g., pencil or marker; slow or medium track)?
- Have I picked a clear stop signal (timer or one playlist)?
- Do I have an aftercare step (tea, walk, call a friend)?
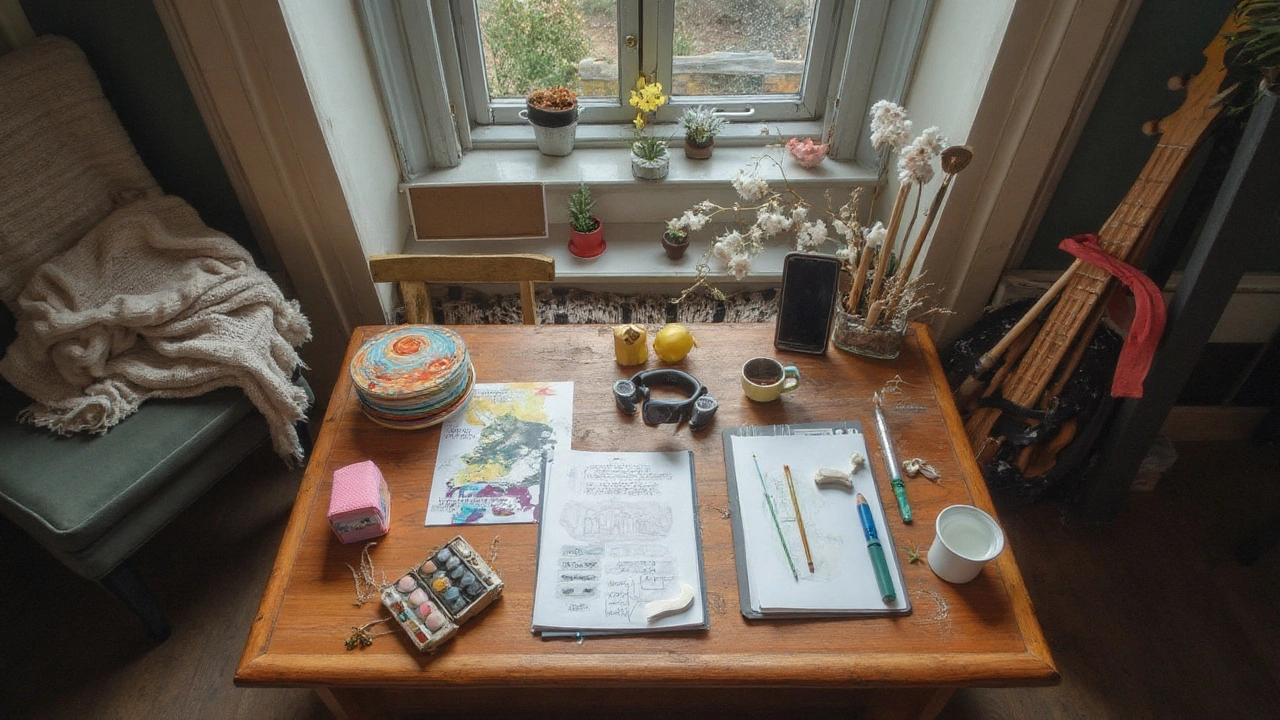
Materials starter kit (cheap and easy):
- Mixed paper, a pencil, two markers, tape, old magazines for collage
- Headphones or a small speaker; a playlist with three tracks in a steady tempo
- Chair with back support; water; a notebook to track mood and sleep
How to measure progress (keep it simple):
- Daily: rate mood, stress, and energy 0-10 before and after your practice.
- Weekly: note sleep quality (short note), social connection (number of meaningful check-ins), and pain ratings if relevant.
- Monthly: list three things that got easier (e.g., “fell asleep faster,” “less Sunday dread,” “walked more”).
Common pitfalls and fixes:
- “I felt worse mid-activity.” Fix: shrink the task (two minutes max), add grounding between steps, and stick to neutral content (shapes, steady beats).
- “I judged my art/singing.” Fix: hide the product, focus on sensation (“smooth, scratchy, soft”), not aesthetics.
- “I skipped sessions.” Fix: attach it to a habit (after coffee), keep materials visible, and set a 10-minute cap.
- “I got triggered.” Fix: stop, orient to the room, name five objects, sip water, and switch to slow exhale breathing. If this repeats, work with a therapist.
Mini-FAQ
- Is this art class? No. The goal is regulation and expression, not skill. If you learn techniques, that’s a bonus.
- How many sessions to feel a shift? Many people notice changes within 4-6 sessions. Bigger goals can take a few months.
- Can I do this if I’m not “creative”? Yes. Start with rhythm and color. They’re the most forgiving entry points.
- Does it replace talk therapy? It can complement or serve as primary care, depending on your needs. Many folks do both.
- What if I have chronic illness or mobility limits? Adapt the activity: seated movement, breath and humming, finger drumming, or visual art with large, easy tools.
- Is it safe for trauma? With pacing and choice, yes. For complex trauma, go slower and consider professional support.
Credentials and ethics (so you can vet providers):
- Training: graduate-level programs, supervised clinical hours, and codes of ethics specific to each modality.
- Titles to ask about: RCAT (art therapy, Canada), MTA (music therapy, Canada), R-DMT/BC-DMT (dance/movement therapy), RDT (drama therapy). Ask about additional counseling or psychology licenses.
- Fit matters: ask how they handle consent, cultural safety, trauma history, and access needs. A good therapist welcomes these questions.
Scenarios and next steps
- If you’re burnt out: pick one 20-minute routine, three days a week, for a month. Protect it like a meeting.
- If you’re managing depression: combine a weekly therapist session with two home practices. Use upbeat music and small, doable art tasks.
- If you live with chronic pain: pair rhythm-based breath with short movement in the morning; top up with music before hard activities.
- If you’re supporting a teen: keep the focus on choice and privacy; let them pick music, materials, or themes. Avoid judging the result.
- If you’re in a remote area: look for telehealth sessions. Art and music adapt well over video.
Troubleshooting by symptom
- Anxiety spike during practice: reduce intensity, pick cooler colors, switch to 4-7 exhale breathing, or shift to low-volume ambient tracks.
- Flat mood and no motivation: start with 90 seconds of rhythmic tapping, then one bright color block. Set a 5-minute timer to get moving.
- Overwhelm with open choices: set micro-rules (“Only circles today,” “Only blue and green,” “Only songs at 70 BPM”). Constraints calm the brain.
- Pain flares: shorten sessions, try chair-based movement, and layer sound at low volume. Gentle pacing beats pushing through.
- Sleep troubles: schedule your practice 60-90 minutes before bed; avoid intense themes at night; finish with slow breathing and soft humming.
How this fits the rest of your care
- With medication: arts therapies can reduce stress and improve adherence. Always discuss changes with your prescriber.
- With physiotherapy: rhythm and movement support gait training and balance; music can boost exercise tolerance.
- With psychotherapy: use art or music to process between sessions, then bring insights to your therapist.
What a good first therapist email looks like (keep it simple):
- Subject: Inquiry about [Art/Music/Movement/Drama] Therapy
- Body: Share your top 1-2 goals, access needs (e.g., seated session), and preferred times. Ask about their approach to consent and pacing.
If you want one change that pays off fast, build a tiny ritual. Same time, same chair, same first song, same pencil. Your nervous system loves predictability. Once that habit sticks, the creative part takes care of itself-and your body learns it can come back to calm, even on rough days.





